Dual eligible special needs plans (D-SNPs) are a type of Medicare Advantage plan designed to meet the specific needs of dually eligible beneficiaries. Originally authorized as part of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA, P.L. 108-173), D-SNPs began operating in 2006. Legal authority was extended several times and made permanent in the Bipartisan Budget Act of 2018 (P.L. 115-123). As of February 2022, D-SNPs were operating in 45 states and the District of Columbia with about 3.8 million dually eligible beneficiaries enrolled (CMS 2022).
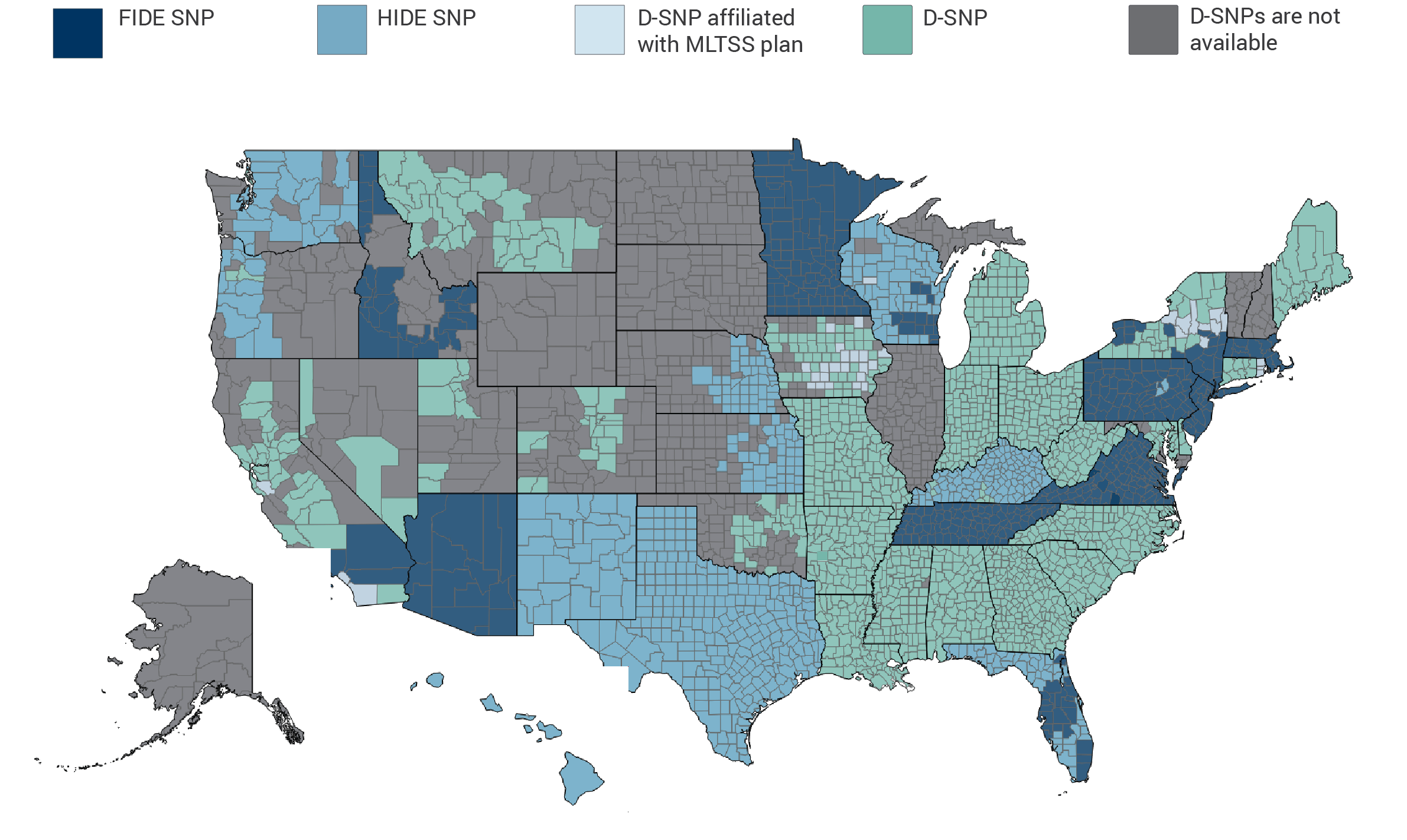
Most Integrated Type of Dual Eligible Special Needs Plan (D-SNP) Available by County, 2021
Notes: The map shows the most integrated type of D-SNP available in each county as of February 2021. Multiple types of D-SNPs may be available in the same county. FIDE SNP is fully integrated dual eligible special needs plan. HIDE SNP is highly integrated dual eligible special needs plan. MLTSS is managed long-term services and supports. D-SNPs are affiliated with MLTSS plans when they are operated by the same parent company. Medicare-Medicaid Plans offered under the Financial Alignment Initiative, not shown on this map, are available in 9 states: California, Illinois, Massachusetts, Michigan, New York, Ohio, Rhode Island, South Carolina, and Texas.
Source: MACPAC analysis of Centers for Medicare & Medicaid Services Medicare Advantage 2021 bid data and state websites.
D-SNPs are required to contract with states but states are not required to contract with D-SNPs (Verdier et al. 2016). The contracts must cover eight minimum MIPPA requirements, including:
- the Medicare Advantage organization’s responsibilities—including financial obligations—to provide or arrange for Medicaid benefits;
- categories of eligibility for dually eligible beneficiaries to be enrolled under the D-SNP, including the targeting of specific subsets;
- Medicaid benefits covered under the D-SNP;
- cost-sharing protections covered under the D-SNP;
- information about Medicaid provider participation and how that information is to be shared;
- verification process of an enrollee’s eligibility for both Medicare and Medicaid;
- service area covered under the SNP; and
- period of the contract.
States have authority under their MIPPA contract to add additional requirements for D-SNPs that further integrate care. Some states have maximized their MIPPA authority and are providing fully integrated care through D-SNPs.
Fully integrated dual eligible special needs plan (FIDE SNP). FIDE SNPs fully integrate care for dually eligible beneficiaries under a single managed care organization. FIDE SNPs were enacted by the Patient Protection and Affordable Care Act (P.L. 111-148, as amended) and permanently authorized, along with regular D-SNPs, in the Bipartisan Budget Act of 2018 (P.L. 115-123). They must have a contract with the state Medicaid agency that complies with the MIPPA requirements above and includes coverage of primary, acute, and long-term services and supports benefits. FIDE SNPs must also cover behavioral health benefits unless the state carves behavioral health out of the capitation rate. FIDE SNPs may be eligible for a payment adjustment to account for the cost of serving a high concentration of frail individuals, depending on their enrollees’ risk scores.
Highly integrated dual eligible special needs plan (HIDE SNP). HIDE SNPs have a higher level of integration than typical D-SNPs. The HIDE SNP designation was created to implement new requirements for D-SNPs that were enacted in the Bipartisan Budget Act of 2018 (P.L. 115-123) and were first made available in 2021. HIDE SNPs must have a contract with the state Medicaid agency that complies with the MIPPA requirements above and includes coverage of long-term services and supports benefits or behavioral health or both.
D-SNP affiliated with managed long-term services and supports (MLTSS). States may integrate care for dually eligible beneficiaries enrolled in their MLTSS programs with D-SNPs. A state that aligns its MLTSS program with a D-SNP typically requires either (1) that the D-SNP operate a companion MLTSS plan or (2) that the MLTSS plan offer a D-SNP. Medicaid MLTSS programs have become more prevalent in recent years. As of November 2020, 25 states operated MLTSS programs, up from 8 in 2004 (Lewis et al. 2018; Advancing States 2020).
For more information on D-SNPs, see MACPAC’s June 2021 report to Congress, Improving Integration for Dually Eligible Beneficiaries: Strategies for State Contracts with Dual Eligible Special Needs Plans.